Health studies and advice conflict with mask marketing
As many move about the country for visits to family and loved ones in the final weeks of 2020 against the cautions of some public officials and health experts, striking images and dismal press portray airports and other travel stations full of people wearing masks. But the same also press masks as the most-essential item. Let’s take a look.
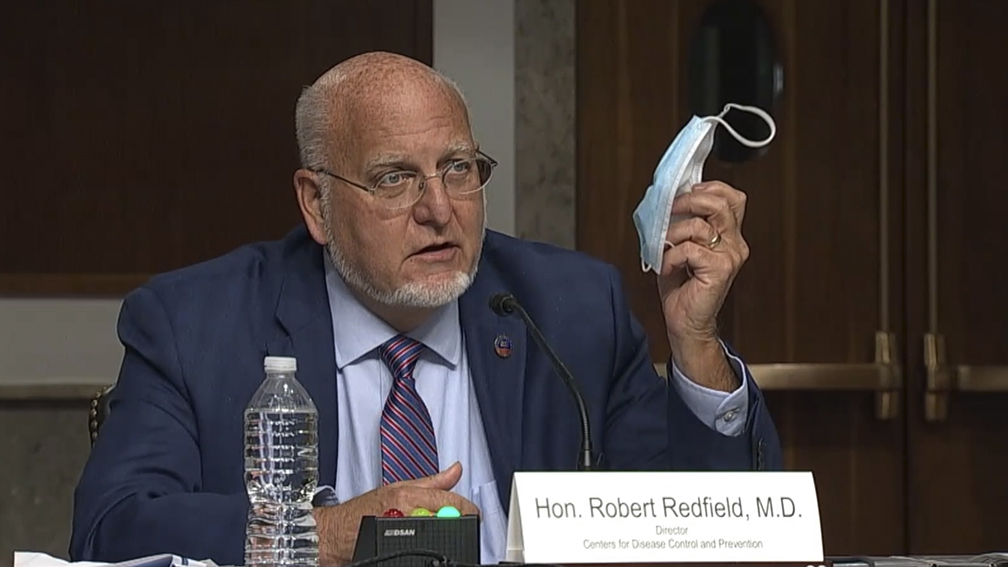
Generally, all press and media marketing focus on masks, presenting them as the most critical factor in preventing the spread of the virus. An off the cuff remark by CDC Director Robert Redfield elevated surgical masks over a quality vaccine, and the media amplified it without evidence. On the contrary, all research and information over the past years have presented clear evidence that other mitigation efforts are more effective than masks. Seeing rising numbers of COVID-19 cases, it is clear that something is not working as it should.
I’ll just say the quiet part loud up-front: masks are not the most important thing you will do to prevent the spread of COVID-19. Despite off the cuff remarks by Redfield, it bears repeating that no study or research has shown masks to be the most important factor in preventing the spread of the virus — physical distancing and hygiene are. Masks, repeatedly throughout vast volumes of legitimate research, have been named as a secondary and even tertiary mitigation action — while media, pundits, and online clout-chasers push masks.
Physical distancing of at least 6 feet is repeatedly found to be the most important thing you can do to prevent the spread of the virus and protect your loved ones from getting sick or dying from COVID-19, according to the top medical research experts in the United States.
Now, we run through information gathered from all available sources, including the American Medical Association (AMA), University of Washington’s Institute for Health Metrics and Evaluation (IHME), the Center for Disease Control (CDC), UC Davis, Hoag Memorial Hospital, and other doctors of infectious disease and epidemiology.
Yes, the marketing that is universally presented is not backed by science. Masks are not the first line of defense, and mask advocates may actually be making the world around us less safe and healthy, instead of more.
By prioritizing masks over social distancing, those marketing health and safety are promoting a lower level of prevention and supporting an environment that is more than 50 percent less-safe in terms of the spread of coronavirus disease. That is a fact, and the results bear out that mask mandates have not been productive in slowing the spread of COVID-19, but instead show correlative and exponential trends toward the inverse of desired results.
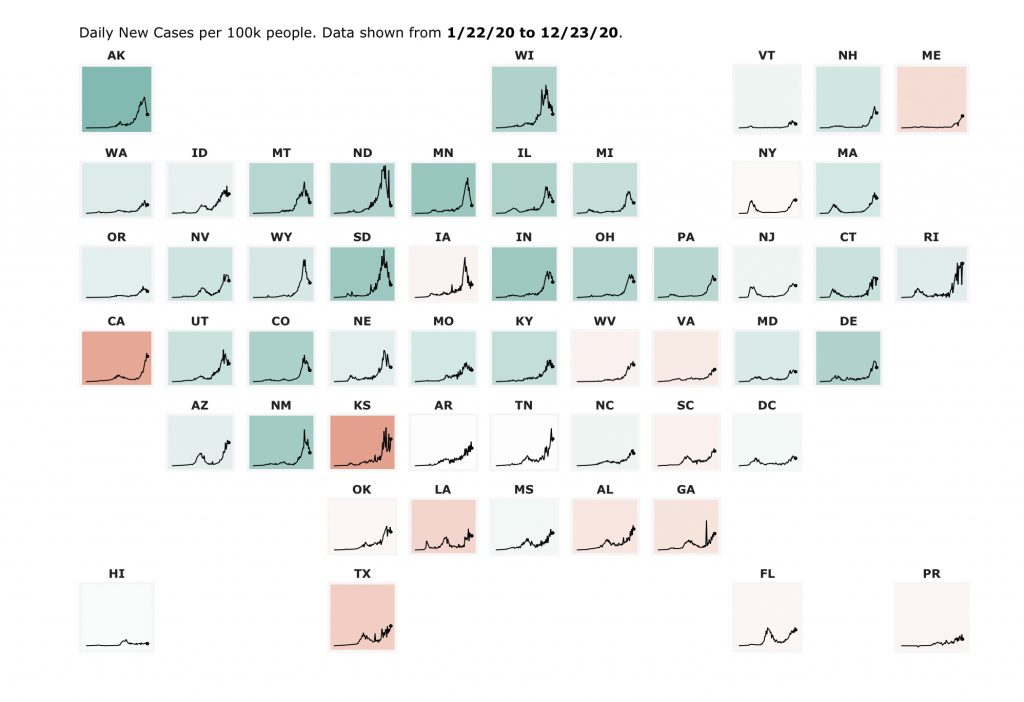
California may be the most outrageous example of mask-wearing and case-increase trending together. According to data collected by Carnegie Mellon University’s CovidCast, California has consistently “masked up,” with the counties of highest case-counts being also the counties with the highest reported mask-wearing.
Some counties report almost 100 percent of people reporting “wearing a mask most or all of the time while in public,” including San Francisco (98%), San Mateo (98%), Marin (99%), Los Angeles (95%), and San Diego (96%). On average, according to Carnegie Mellon University, California as a whole has reported about 95 percent mask usage on average over the past three months. So why are cases continuing to increase at the nation’s most rapid rate?
It is likely because, according to doctors at UC Davis, masks help reduce spread up to 65 percent while distancing of six feet or more is 90 percent effective. At a much lower rate, IHME claims masks reduce spread by only 30 percent.
According to all recent reports, the spread of COVID-19 is occurring in social gatherings, including family gatherings, and this is a case where masks might not be helpful at all.
According to experts at the Indiana University, masks are not a replacement for social distancing. The university’s assistant director of public and environmental health for IU Environmental Health and Safety Graham McKeen said, “Wearing a mask also does not mean that we should stop or ease physical distancing … physical distancing is the best tool we have.”
In contrast, media outlets and even public health agencies are not prioritizing distancing in messaging and reporting.
On Dec. 14, CNN medical analyst and emergency physician Dr. Leana Wen stated “those who get the vaccine should still be wearing masks and practicing physical distancing,” in an article titled “Why a Covid-19 vaccine doesn’t mean you can stop wearing a mask.”
The headline is about masks, and Wen prioritizes masks before distancing in her verbalized answer. All the studies worldwide have shown that distancing is the most effective tool, and not a single study has proven that masks are a solid measure absent additional measures of distancing and washing hands.
Not the AMA, CDC, IHME, or any medical experts have produced studies or pointed to studies that evidence masks as a preventative measure that competes in efficacy with distancing and hygiene.
Wen is not the only one misrepresenting the effects of masks. In September, the Director of the CDC, Robert Redfield contradicted his own agencies posted guidance when he famously held up a mask while testifying before a Senate committee and said “I might even go so far as to say that this face mask is more guaranteed to protect me against COVID than when I take a COVID vaccine.”
He later told the Senate committee that “These face masks are the most important, powerful public health tool we have. And I will continue to appeal for all Americans, all individuals in our country, to embrace these face coverings. I’ve said if we did it for 6, 8, 10, 12 weeks, we’d bring this pandemic under control.”
Redfield seemed to shoot from his hip when making the claim without supporting research, unless he was speaking specifically about the sociological element of masks instead of the epidemiology. The fact that Californians are using masks heavily at higher than 95 percent over the past 12 weeks while seeing exponential rise in cases argues he is wrong about his assumption — which again, he stated without supporting evidence or research.
The top guy at the CDC making such statements on a political stage is just one of the PR blunders plaguing the CDC over the past year, including “accidentally” posting that the virus had gone airborne to their website and then quickly removing and dismissing as a “draft.” (Why the CDC is drafting patently wrong information on their website is curious, to say the least.)
He later tweeted about the importance of the vaccine, and added “The best defense we currently have against this virus are the important mitigation efforts of wearing a mask, washing your hands, social distancing and being careful about crowds.”
See again that even Redfield’s emphasis when speaking about the “trifecta” of slowing the spread, he prioritized masks, despite there being no evidence that they should be seen as the most effective prevention.
On top of that, the damage was done, as media outlets ran headlines like “CDC director suggests face masks offer more COVID-19 protection than vaccine would” from CBS News and CNBC.
In that article, CBS News quoted George Rutherford, a professor of epidemiology and biostatistics and director of the Prevention and Public Health Group at UC San Francisco, who said the CDC director is “completely right.”
Rutherford went on to claim that masks may be 95 percent effective and the vaccine only 80 percent effective, without referencing any evidence for either claim. This misinformation by a professor at UC San Francisco then makes its way into mainstream conversations from what would sound like a credible source but lacks evidence for such a claim. He may have been referring to the N95 mask, which is designed to block 95 percent of small particles, but Redfield was specifically holding a surgical mask, known to be far less effective. Also known is that the N95 mask protects the wearer, but the valve allows for the release of droplets, with no protection for others.
In April of 2020, UC San Francisco compiled a manuscript named “Face Masks Against COVID-19: An Evidence Review” which only regarded face masks as “valuable” when used “in conjunction with widespread testing, contact tracing, quarantining of anyone that may be infected, hand washing, and physical distancing.”
The manuscript was a study of dozens of research papers on the topic, which referenced 96 different studies on a variety of viruses, masks, and sociological behaviors.
But claims of certainty in the manuscript were avoided. Instead of certainty about the disease, there was a sociological assumption that masks could simply signal for higher compliance to the more effective measures, such as distancing and hand washing.
Like Redfield said, masks are a “powerful public health tool,” which may refer to sociological compliance more than epidemiological health, as the UCSF manuscript detailed.
“Another important benefit of recommending universal mask-wearing would be to serve as a visible signal and reminder of the pandemic, and given the importance of ritual and solidarity in human societies, it is plausible that visible, public signaling via mask-wearing can potentially increase compliance with other health measures as well, such as keeping distance and hand-washing,” the UCSF manuscript noted.
There is certainly nothing wrong with that signal, but an “important benefit” of a mask having nothing to do with infection rates should be framed as such. Left to public discourse, misrepresenting information leaves the door open to skepticism and even conspiracy theories about intent. If 2020 has proven anything, it is that blind faith in institutions is no longer a credible factor in public policy, and when “experts” disagree wildly, it inspires debate instead of compliance.
The manuscript noted other sociological anecdotes like “Mask-wearing and even mask-making or distribution can provide feelings of empowerment and self-efficacy, which would in turn also suggest masks could increase compliance in other health-behaviors as well by increasing self-efficacy,” which by themselves are not without value, but don’t speak to the prevention of spread of COVID-19.
Of studies on the efficacy of masks, like those referenced in the UCSF manuscript, and The Lancet study in June, showed that while N95 masks were more effective than cloth and surgical masks, it reported “low certainty” for a “result in large reduction in risk of infection” for mask usage.
This makes it difficult on those of us who want to “follow the science” and “trust the experts” because they are not saying the same things. However, research continues to say the same thing: distancing (of 6-feet or more) is the most effective action that can be taken to reduce the spread of COVID-19.
According to the American Medical Association, “Social distancing is said to be the best way to stop the spread of the virus.”
Meanwhile, crowds gathered for protests and rallies over the year — from Black Lives Matter, anti-lockdown, Trump campaign rallies and parades, and election results rallies post-Nov. 3 — and like a warm blanket, the social and mainstream media was quieted by continued claims that “at least people were wearing masks.” Meanwhile, cases increase along with mask usage, coincidentally.
That isn’t actually too surprising. Both research and epidemiological science suggests that masking was not all that effective. Despite more than 95 percent mask usage in California, we see higher cases, more hospitalizations, and more COVID-19 related death.
According to the University of Washington IHME, “universal mask use” is projected to be the most-effective against longterm death tolls, with the “target” rate being 95 percent — however, California’s running average is slightly higher than that to little evidence it is working. Surrounding states of Oregon (94), Nevada (94), and Arizona (93) show nearly 95 percent mask usage, so it is not that California is being harmed by neighbors nor lack of masking up.
The possibility that masking being so heavily promoted is creating a lax in more effective measures.
In research produced on Oct. 30, the CDC found that people were more likely to wear masks than distance. That would explain why cases are rising, as masking is less-effective than distancing, according to all sources referenced here.
So now what? People will do what they do. Mandating tyrannical and oppressive measures is not congruent with the values in the Constitution of the United States or the California Constitution. The Supreme Court has consistently ruled not to suspend the constitution, and it has proven to be an irreconcilable public argument in the face of a disease with a recovery rate of better than 95 percent, an average age of death of around 80-years old and a 2.6 co-morbidity factor.
Economic closure and mask mandates from state to state show no consistency in results that either is a significant factor. States with vastly different approaches show similar trend lines, and states with similar approaches show variant trends. This flies in the face of ardent claims that a unified federal mandate would have been effective from President Trump’s administration. Seriously, ask yourself honestly if Trump had rolled out a heavy-handed mandate, do you really think people would have paid more attention? In my opinion, it would only have satisfied the authoritarians among us, with no real impact. I certainly would not have taken a Trump mandate any more seriously than a Newsom mandate. But that is just me.
The right thing to do is stay healthy. Health experts agree that diet and exercise are dominant factors in maintaining health. Staying indoors for some is not a healthy ingredient, so people will move around and live life outside.
There is no science blaming the spread of COVID-19 on people not wearing masks, but there is science showing that the most effective thing we can do is distance at 6-feet or more, even with people we see regularly, and sanitize our hands and clothing. Sanitization kills the virus, and studies also suggest that mouthwash may also kill the virus.
People wearing masks are getting COVID-19, and spreading COVID-19. In the midst of the most aggressive spike in cases since the start of this crisis, something is obviously missing from the effort. Experts agree.
“As far as face masks versus social distancing by at least 6 feet, the face masks do not replace social distancing,” said Peter Gulick, an infectious disease specialist and professor of medicine at Michigan State University.
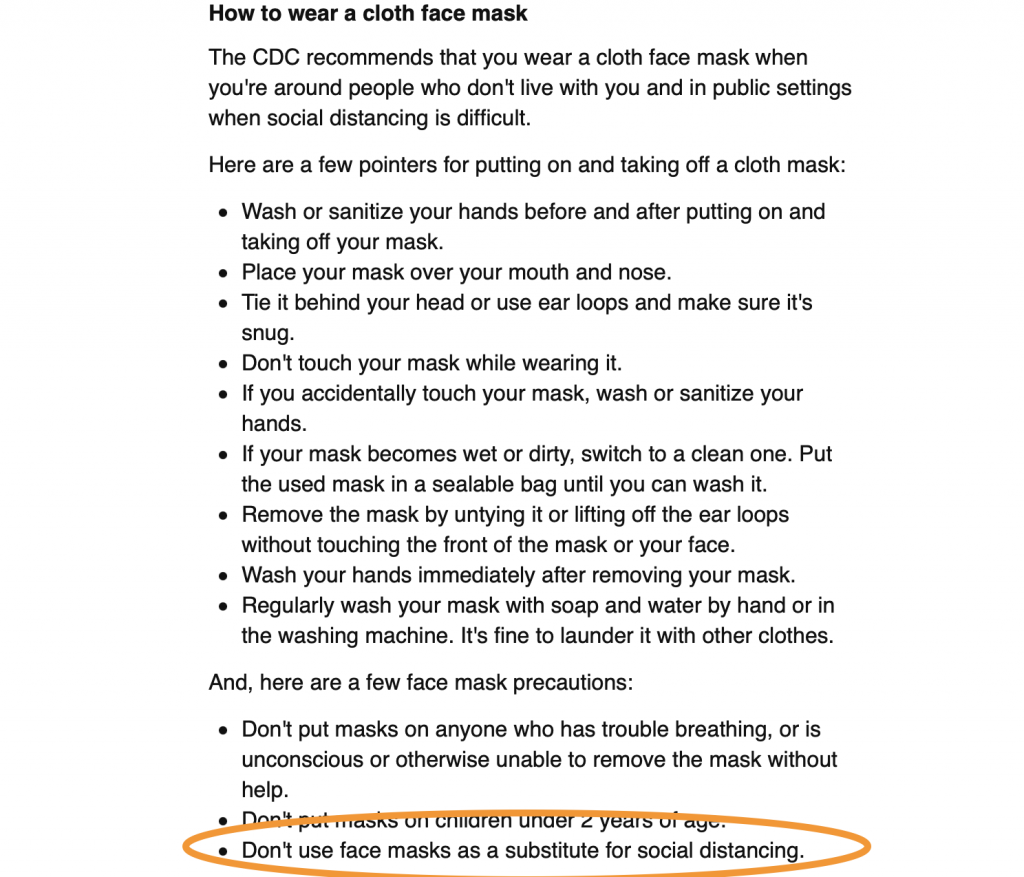
On the CDC website, updated Dec. 18, the information reads, “A mask is NOT a substitute for social distancing. Masks should still be worn in addition to staying at least 6 feet apart, especially when indoors around people who don’t live in your household.”
A study by the National Bureau of Economic Research in October warned about face mask compliance leading to a decrease in distancing and rising infections.
In the introduction to the working paper “Face Masks, Public Policies, and Slowing the Spread of COVID-19: Evidence from Canada,” it stated that “a face mask mandate may not be effective in practice … if it leads to increased contacts due to a false sense of security.”
Ashley Luckman, a research fellow at Warwick Business School and lead author of the study said, “If the government’s aim is to minimize transmission of the virus, its guidelines must be clear enough to prevent this trade-off, emphasizing that masks are not an alternative to social distancing.”
Yet we continually hear from our local agencies, municipalities, government officials, and other media outlets that it will all get better if we wear more masks. None of the data has shown this to produce a desirable outcome or be consistent with true care for the health of one another and the survival of our most vulnerable.
It isn’t that masks don’t work. It is that they don’t work very well, and they certainly by all health measurements don’t work as well as distancing and sanitization, especially when a mask is not sanitized regularly. It’s a visual that signals some measure of care and sensitivity, but anyone serious about slowing the spread will acknowledge that all the studies, both laboratory, case, and epidemiological, have shown that distancing is the most important, and that masks are a tertiary mitigation.
As opposed to “Wear a Mask, Wash your Hands, and Keep 6-feet Distance” the mantra is corrected, epidemiologically, as, “Keep 6-feet Distance, Wash your Hands, and Wear a Mask” in that order of efficacy.
With all the data available, it is evident that anyone serious about slowing the spread and saving lives will place distancing as the priority, and acknowledge what the experts have repeatedly stated, that masks are not a replacement, and are not as effective in slowing the spread of COVID-19.
Watching scores of video of election-related segments with officials giving interviews there is an exorbitant amount of mask adjusting by people, more face touching than is usual for people during conversation, which concerns oral transmission of the virus by speaking into a cloth mask, touching it with bare hands then shaking hands with others or touching common areas such as door handles, etc.
In conclusion, this is not medical advice nor intended to persuade action, but to think, ask questions, and encouragement to discuss specifics with a doctor of medicine, especially infectious disease. The marketing departments are the business end, but if we are going to make a difference in an epidemiological situation, we should follow the best science until better science prevails. If results were desirable, I’d say keep up the good work, but as things stand, maybe we are doing something wrong. The research says we are.
Ultimately, we are only in control of a small part of the world, and staying clean is a factor in any disease control effort. Personal health and strong immune response is another means of personal protection. Do what fits your personal lifestyle, and ask more questions.
For yourself and loved ones, to ensure the highest level of health and safety in prevention of the spread of COVID-19, follow the science and instructions supported by science: keep a distance of 6-feet or more from people outside your residence; wash your hands regularly; and wear a clean mask when near other people outside your residence.
Knowledge is the antidote of fear. We know a great deal about how to prevent spread of the novel disease. Pay attention to who is prioritizing masks over time-tested science. Once you see it, you can’t unsee it.
While the evidence correlates mask usage and the current spread of the virus, there is no studies yet to connect the two. All we know at the moment, is wearing masks is not stopping it. The marketing of masks has planted unproven ideology that people who are not wearing masks are causing the outbreak, but in California where more than 95 percent have been wearing masks, especially in urban areas, this simply does not comply with the evidence.
It is my opinion that those who prioritize masks as a preventative measure above distance and hygiene are not serious about slowing the spread or saving lives — or they simply haven’t looked at the research. Masks work when combined with distance of more than 6 feet and good personal hygiene.